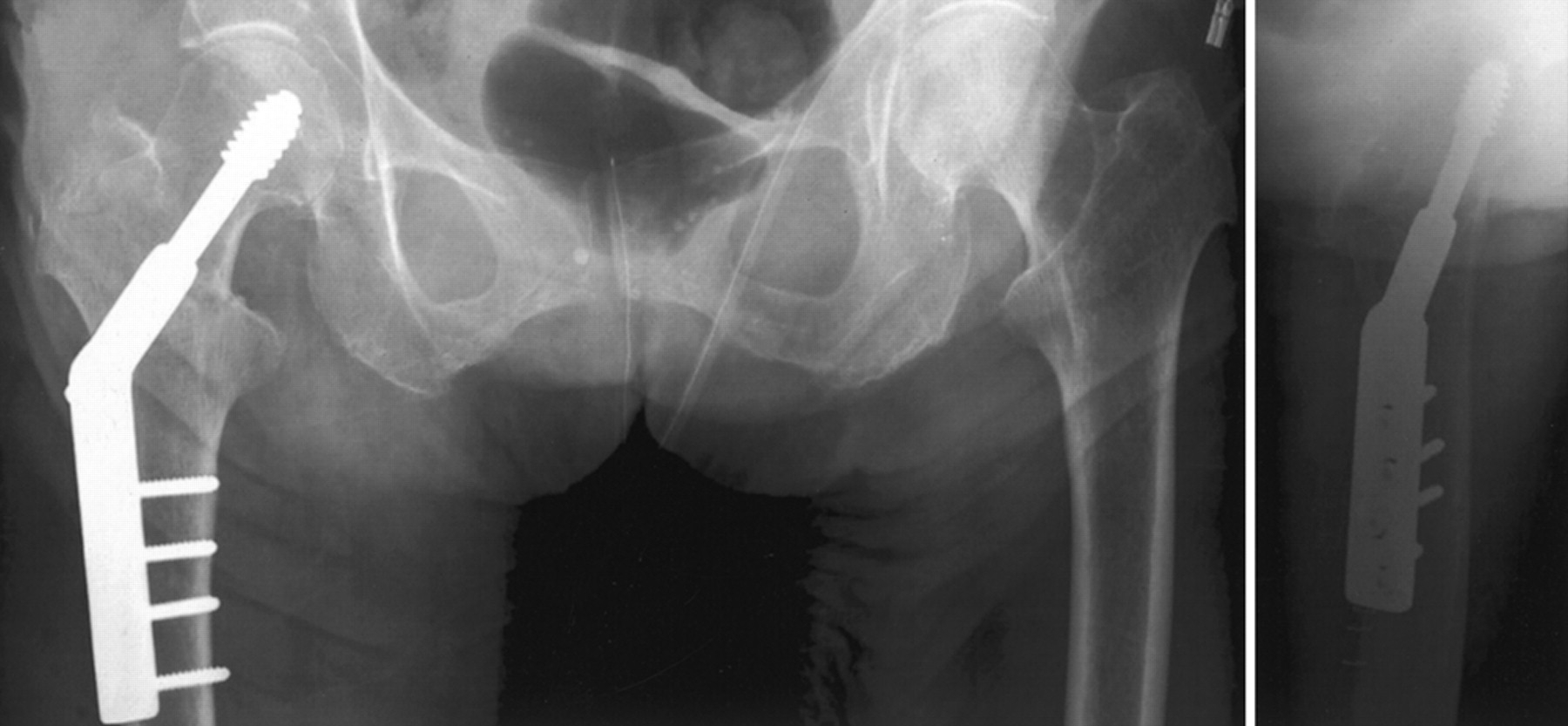
Dynamic Hip Screw (DHS) technique is straightforward to learn and frequently comes up at ST3 Trauma and Orthopaedic Interviews.
It is important that you know the steps, kit and can talk through the procedure while performing the steps on a saw bone. Check out our sample questions for the quick DHS kit spot test.

Before getting started with how to do it lets just recap the importance of the position of the lag screw.
- Indications
- Pertrochanteric fractured neck of femur
- When to use a nail:
- Reverse oblique proximal femoral fracture
- Sub-trochanteric femoral fracture
The Procedure
Opening statement: In an appropriately marked, consented and WHO-cehcklisted patient I would...
Pre op Requirements
- WHO Team brief (equipment i.e traction table)
- Antibiotics as per trust protocol
- Image Intensifier
Positioning
- Supine on traction table
- Remove triangle from under operated buttock
- Position post between legs and bring patients perineum down to post
- Operated leg onto traction
- Non-operated leg into a lithotomy position (compression stockings, and calf compression device)
- Patient warming
- Arms strapped across chest and away from potential harm from image intensifier C-Arm
Fracture Reduction Technique
- When reducing the fracture apply inline traction and turn the patella to face the ceiling. Check this against the image intensifier and apply more/less traction and internal/external rotation of the hip as required.
- Reduction is assessed on the:
- AP view
- Fragments reduced to acceptable position
- Length – restoration of shentons line
- Varus / valgus angle (should be around 135degrees)
- Lateral view
- Alignment of shaft, trochanters and neck
- AP view
Technical considerations
- Baumgaertner et al. published in the Journal of Bone and Joint Surgery America in 1995 their paper describing the cut out (failure rate) of DHS screws in consideration to tip apex distance (which should be less than 25mm) and the position of the lag screw in the head (should be AP centre / Lateral centre).
The Procedure
Dissection
- The operative technique can be found here
- Prep and drape the operated limb (Anterior Superior Iliac Crest to knee), then use clear sticky drape and place over bar and stick down
- WHO safer surgery check prior to skin incision
- Image intensifier to approximate entry point and incision
- Palpate the femur and make your incision cutting through, skin, then subcutaneous fat, then down onto fascia lata
- Incise the fascia, then use the scalpel/scissors to split the fascia proximally and distally
- You can then either use a vastus splitting or vastus-elevating approach to the femur
- Use a Bristow elevator to sweep the vastus off the bone
- Place a Norfolk and Norwich retractor (handle pointing to toes so it doesn’t interfere with you II imaging) to retract vastus lateralis
Guide Wire Position
- Take the 135 degree jig and 2.5mm DHS wire
- Position the jig onto the femur and take an AP image of the hip with the II machine (generally the ideal entry point tends to be at approximately the level of the lesser trochanter)
- On the AP view advance the wire a few of centimeters (remember that the femoral neck is anterverted so you need to drop your hand towards the ground to aim the tip of the wire up about 15 degrees)
- Check the lateral view with the II to ensure that the guide wire is heading to the centre of the head on the lateral view
- Once happy with the position of the wire advance under II control until approximately 5mm away from the cortex of the femoral head in the AP and Lateral view
- Measure the length of the wire (usually around 95mm), if less than 80mm use short barrelled DHS plate
Reaming
- Set triple reamer to the length of the screw
- Ream under II control taking frequent radiographs to ensure that the guidewire is not advanced into the pelvis
- Remove reamer, leaving guidewire in the bone (if the wire is removed ensure that its position once reinserted is checked with II)
Insert Screw
- Insert screw using centralising guide on screw driver, screening whilst inserting (basicervical type of fractures can sometimes displace whilst inserting the screw, therefore ensure you screen with II. If the fracture starts to displace back the screw out slightly and insert an additional wire above the screw to act as a de-rotational wire and stop the head from moving)
- Once screw is inserted ensure that handle is parallel to the femur to allow the plate to slide on
Apply Plate
- Select a 4-hole DHS plate
- Ensure it is sitting flush on the femur
- Use the plate impactor to push DHS plate onto bone
- Use a 3.2mm drill bit and universal drill guide to drill the distal hole (ensure that sitting fully on bone)
- Measure screw hole and insert screw
- Ensure sitting on bone correctly
- Remove guidewire
- Drill, measure and insert the remaning screws
Closing
- Take AP and lateral of the femoral neck and head, and AP and lateral views of the plate on the femur with the II machine and save them and upload them onto digital x-ray system
- Washout wound
- Ensure adequate haemostasis
- Closure (1 vicryl to muscle and fascia, 2/0 or 0 vicryl to subcutaneous fat, 3/0 monocryl to skin)
- Occlusive dressing over wound or skin glue
- Ensure safe transfer of patient off the traction table
Post op
- Check Haemacue in recovery
- Monitor observations / urine output & neurovascular status of the limb
- Check HB, U&Es mane
- Mobilise Full Weight Bearing as pain allows
- VTE prophylaxis as per hospital policy
- Removal of sutures if necessary
- No routine follow up usually required
Further Resources