The BOA Standards for Trauma (BOAST) Guidelines are extremely useful when preparing for ST3 Trauma and Orthopaedic Interviews. It is vital to know each in detail and how to apply these in an orthopaedic interview clinical case.
BOAST 1 - Patients sustaining a fragility hip fracture
Over 70,000 hip fractures occur annually in the UK. The total cost of care is over £2 billion with 10% mortality at 30 days and up to 30% mortality at one year. Their care is dependent on close multidisciplinary relationships between many specialities due to the complex nature of these patients, both in terms of their medical co-morbidities and their ability to rehabilitate.
BOAST 2 - Spinal clearance in the trauma patient
All patients involved in significant blunt trauma must be assumed to have an unstable injury to their spine; the incidence is approximately 2% and increases up to 34% in the unconscious patient. 50% of spinal injuries occur in the thoracic or lumbar spine; 20% at two levels. Immobilisation with full spinal precautions for prolonged periods creates difficulties in intensive care units. Spinal immobilisation is associated with pressure sores and pulmonary complications and is not recommended for more than 48 hours. Audits in the UK suggest poor implementation of spinal clearance policies. In the neck ligamentous disruption without a major bony injury may lead to instability.
BOAST 3 - Pelvic and acetabular fracture management
Major pelvic and acetabular fractures must be managed with an established trauma system with defined referral pathways. A mismanaged pelvic injury can lead to early death from haemorrhage or major disability while delayed or poor management of an acetabular fracture can lead to accelerated osteoarthritis and avoidable permanent hip dysfunction. 5-10% of pelvic fractures will have a major urological injury. The major fracture incidence has been estimated at 3 displaced acetabular fractures per 100,000 population per year.
BOAST 4 - The management of severe open lower limb fractures
The British Orthopaedic Association and the British Association of Plastic, Reconstructive and Aesthetic Surgeons have reviewed their 1997 guidance and now publish a review of all aspects of the acute management of these injuries using an evidence-based approach, leading to the “Standards for the Management of Open Lower Limb Fractures,” which are free to download from www.boa.ac.uk and www.bapras.org.uk. This BOAST is derived from these standards. Contrary to traditional teaching, best outcomes are achieved by timely, specialist surgery rather than emergency surgery by less experienced teams.
BOAST 5 - Peripheral nerve injury
All surgeons undertaking Musculoskeletal Trauma Surgery will be involved in the management of peripheral nerve injury, either as a result of injury or a postoperative complication. Nerve repair and complex nerve injuries (e.g. brachial plexus) is now a specialist field but all surgeons involved in trauma surgery must be able to diagnose nerve injuries and identify those that need referral to a specialist. These audit standards have been distilled from the recent BOA blue book on peripheral nerve injury which provides evidence-based guidelines for management.
BOAST 6 - Management of arterial injuries
Arterial injuries to the extremities are rare and present a diagnostic and management challenge if limb salvage is to be successful. In civilian practice, fast and accurate diagnosis is of paramount importance. There should be immediate referral to a surgeon with the skills to perform vascular repair. A low threshold for early surgical intervention is important for successful salvage. The responsibility for managing these cases lies jointly with the orthopaedic surgeon and the team managing the vascular injury.
BOAST 7 - Fracture clinic services
These guidelines are for the standard of care patients should expect following significant, acute soft tissue or bone injury that requires specialist treatment from a Trauma and Orthopaedic Surgeon in the outpatient setting (fracture clinic). They provide standards that can be audited to evaluate the quality of an outpatient fracture service. They cannot be comprehensive as local facilities and geography will require variation in the configuration of these services. However, the British Orthopaedic Association believes that these are the care standards that all patients in the United Kingdom can expect.
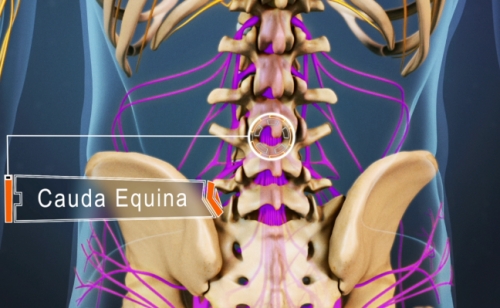
BOAST 8 - The management of traumatic spinal cord injury
Spinal cord injury resulting in neurological deficit is a rare but potentially devastating injury. Compromise to the spinal cord may be due to trauma, vascular injury or other disease process and can result in immediate or insidious onset of neurological symptoms including loss or reduction of voluntary motor function, sensory impairment, bowel or bladder dysfunction and loss of autonomic function. The incidence in the United Kingdom is estimated at 12-16 per million population with about 75% of cases due to trauma. Appropriate management from the time of diagnosis of cord injury has been shown to have significant effect on the long-term outcome for patients and reduce short and long-term complications.
BOAST 9 - Fracture liaison services
Fracture Liaison Services (FLS) provide secondary prevention for fragility fractures (defined as a fracture following a fall from standing height or less). These services systematically and proactively identify patients in secondary and/or primary care who have suffered a fragility fracture and assess the patient’s risk of future fragility fracture in a timely fashion. FLS then provide advice and/or therapy to reduce that risk. There is now good evidence that these services are cost-effective and can result in a reduction in the incidence of fragility fractures in the local population.
BOAST 10 - Diagnosis and management of compartment syndrome of the limbs
Acute compartment syndrome of a limb is due to raised pressure within a closed fascial compartment causing local tissue ischaemia and hypoxia. In clinical practice, it is most often seen after tibial and forearm fractures, high-energy wrist fractures and crush injuries. Other important causes include restrictive dressings or casts, prolonged immobilization and reperfusion of ischaemic limbs. Early diagnosis and treatment is vital to avoid severe disability. Pulses are normally present in compartment syndrome. Absent pulses are usually due to systemic hypotension, arterial occlusion or vascular injury.
BOAST 11 - Supracondylar fractures in the humerus in children
Supracondylar fractures of the distal humerus are the most common fractures about the elbow seen in children. They may be difficult to manage and can be associated with significant complications including nerve injury, vascular compromise, malunion and compartment syndrome.
BOAST 12 - The Management of Ankle Fractures
Ankle fractures are common and the majority are the result of low energy torsional trauma. The aim of treatment is to restore and maintain stability and alignment of the joint, ideally with normal anatomy of the ankle mortise. This should optimise functional recovery and reduce the chance of development of post-traumatic arthritis.
BOAST 13: Rehabilitation and Communication with Trauma Patients
Rehabilitation is the process of restoration of a patient to their pre-injury state. A rehabilitation Prescription starts by identifying the components of the injury and the interventions required. These interventions may include acute management, surgery and therapies. Trauma can be a sudden and life changing event that may have a devastating effect on patients, their families and friends. Since the advent of trauma networks, the most appropriate care may require transfer and treatment away from the nearest hospital. It is recognised that recovery from injury requires multidisciplinary coordinated care including good communication and rehabilitation from the time of injury.
BOAST 14: The Management of Urological Trauma Associated with Pelvic Fractures
Urological trauma is rare and the incidence of severe urethral trauma is 1/million population/year. The majority of cases are due to blunt high-energy trauma with associated multi-system injuries and 80% of these cases are associated with pelvic fractures. Urological injuries are potentially fatal and can result in severe long-term disability.