Lisfranc Injury
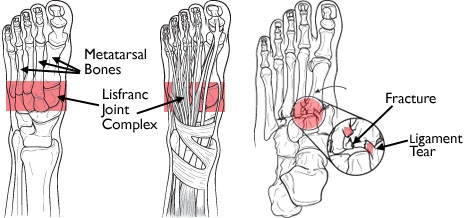
The tarsometatarsal joints are collectively known as the "Lisfranc joint" after the Baron de Lisfranc, a Napoleonic army surgeon who described an amputation through the foot at this level. "Lisfranc injury" refers to a group of bony and/or soft tissue injuries which affect the tarsometatarsal and sometimes other midfoot and forefoot elements.
Anatomy
In transverse section, the metatarsal bases form part of an arch, with the bones wider above than below to fit the arch. The strongest part of the arch is the 2nd TMT joint, which is recessed into a mortise between the medial and lateral cuneiforms. The plantar ligaments are stronger than the dorsal ligaments, and are reinforced by the plantar fascia and intrinsic muscles. The strongest ligament of all is the Lisfranc ligament between the medial cuneiform and the base of the second metatarsal.
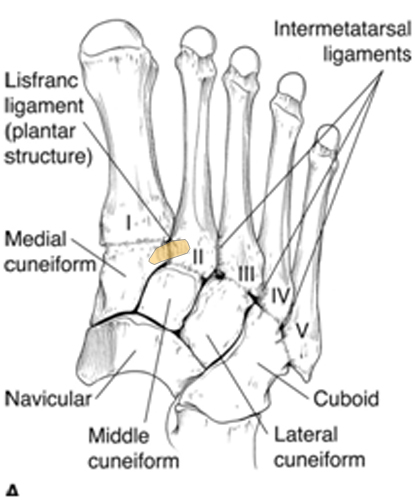
Typical and severe Lisfranc injuries have extensive ligament disruption and fractures. Recently a "subtle Lisfranc injury" has been described, a category in which displacement of the TMT joint is minimal and may only be apparent on loading. Panchbhavi (2008) shed light on the biomechanics of such injuries. In a cadaver study, Panchbhavi found that instability on simulated end-stance loading could be created simply by dividing the Lisfranc ligament. The instability consisted of abnormal rotational movements between the medial cuneiform and second metatarsal.
Imaging
AP, lateral and oblique radiographs are required. Weight-bearing views are key as weight-bearing allows for visualisation of any functional instability. The degree of dorsal or plantar displacement may be apparent only on the lateral film. CT may be useful to assess more complex injuries and Lu et al (1997) showed that CT is better than plain radiography on assessing minor incongruity.
There are five critical radiographic signs that indicate presence of midfoot instability:
- disruption of the continuity of a line drawn from the medial base of the second metatarsal to the medial side of the middle cuneiform
- widening of the interval between the first and second ray
- medial side of the base of the fourth metatarsal does not line up with medial side of cuboid on oblique view
- metatarsal base dorsal subluxation on lateral view
- disruption of the medial column line (line tangential to the medial aspect of the navicular and the medial cuneiform)

Management
Undisplaced “subtle Lisfranc injuries” may resolve with casting and non-weightbearing, probably for about 8 weeks to allow the ligaments to heal. However, there is a risk of displacement and we would recommend percutaneous screw fixation of these injuries.
Operative Intervention
The TMT joints are usually accessed through longitudinal incisions designed to give access to as many rays as necessary, to be extensile and to protect the intervening skin bridges. A single incision can give access to the 1st and 2nd rays and another to the 3rd, 4th and 5th or a medial or dorsomedial approach can give access to the first ray, another to the 2nd/3rd and another to the 3rd/4th. A transverse dorsal approach has been described (Vertullo 2002).
Some Lisfranc dislocations can be reduced closed and stabilisation achieved with percutaneous screws, but most require formal open reduction.