Core Knowledge: Supracondylar Fractures
29/10/13 04:36 Filed in: Core Knowledge | Wednesday Blog

Today’s Wednesday Blog gives looks at a common ST3 orthopaedic interview clinical question: paediatric supracondylar fractures.
Background
Supracondylar fractures make up >60% of paediatric elbow fractures. Extension type injuries are more common (80-95%) than flexion type.
Associated injuries are important:
Anterior interosseous nerve (branch of median n.) neuropraxia
- the most common nerve palsy seen with supracondylar humerus fractures
Radial nerve palsy
- second most common neuropraxia (close second)
Ulnar nerve palsy
- seen with flexion-type injury patterns
Nearly all cases of neurapraxia following supracondylar humerus fractures resolve spontaneously, and therefore, further diagnostic studies are not indicated in the acute setting. For those that persist in the acute setting allow 2-3 months for them to resolve with follow up.
Vascular injury (1%)
-Brachial artery, rich collateral circulation can maintain circulation despite vascular injury
Anatomy
The time of fusion of the ossification centres of the bones around the elbow seen on AP and lateral radiographs correspond to age as below:
Mnemonic: CRITOL
Capitellum 2 years
Radial head 4 years
Internal (medial) epicondyle 6 years
Trochlea 8 years
Olecranon 10 years
Lateral epicondyle 12 years
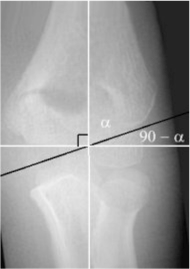
Baumann’s angle is the angle between the lateral condylar physis and the long axis of the humerus shaft. After reduction and fixation, Baumann’s angle should be equal to that of the uninjured side (usually 70–75°). More than 75° denotes varus malposition. Correct rotational alignment is best judged on a lateral view x-ray. Alpha in the image below is Baumann’s angle.
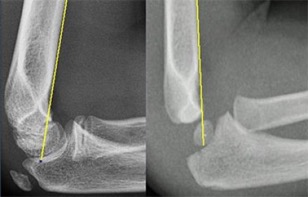
The anterior humeral line on lateral XR should intersect the middle third of the capitellum. The capitellum moves posteriorly to this reference line in extension type fracture.
Classification
Gartland (1959) classifies supracondylar fractures by displacement and cortical contact.
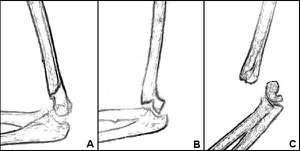
Type I
Undisplaced or minimally (<2mm) displacement with anterior humeral line intact
Type II
Displaced >2mm, anterior humeral line no longer passes through centre of capitellum but posterior cortex is in contact
Type III
Displaced with periosteum torn and no cortical contact
Type IV (modified)
As type III but unstable in flexion and extension
Management
Full history and examination.
In young children asking them to copy your hand movements is useful:
- ‘ok’ sign for AIN
- cross middle over index finger for ulna
- flex wrist or MCPJ for radial
The NV status should be documented in ED and an above elbow backslap applied in 40 degrees of flexion.
Pale, pulseless hand
Approximately 10-20% of Gartland III fractures present with an absent pulse. As the hand is also pale the circulation is not maintained by the collateral supply and emergent (immediate) reduction of the fracture is required with percutaneous pinning. An arm that is pulseless with poor perfusion is an emergency.
From the literature reduction and fixation restores the pulse in the majority of cases (75%) with the artery in spasm or trapped in the fracture site. If the pulse is not restored following reduction and percutaneous pinning open exploration of the artery is required with the vascular team.
Pink, pulseless hand with nerve injury
In this case the rich collateral blood supply maintains circulation to the hand despite vascular injury. An absent radial pulse is not in itself an emergency as the collateral circulation keeps the arm perfused.
There is some controversy in the literature as to the most appropriate course of action. Presently urgent but non-emergent reduction and pinning is advised though more recent studies suggest a concurrent nerve injury may indicate a co-existing vascular tethering at the fracture site due to the proximity of vessels advising immediate reduction and early exploration to untether vessels if the pulse does not return.
Pink, pulseless hand without nerve injury
This remains the most controversial area in the literature. Urgent but non-emergent reduction and fixation is required
If the pulse does not return after surgery but the hand remains perfused most centres advocate monitoring the patient for 48 hrs. If the hand becomes pale exploration is then required with the vascular team.
In practical terms most supracondylar injuries present towards the end of the day and provided the patient is starved fixing them in twilight hours is sensible.
Reduction Technique
The below steps summarise the reduction manoeuvre:
- Traction: disengages the proximal fragment from the brachialis muscle
- Coronal plane correction: medial or lateral translation
- Axial plane correction: correction of internal rotation deformity
- Distal fragment reduced: push with thumb on olecranon
- Elbow flexion >100°
- Pronation: tightens medial periosteal sleeve
If the fracture is difficult to reduce prolonged traction (10-20minutes) may be necessary to help disengage the proximal fragment from the muscle pull. An alternative in a non-emergent reduction is to keep the patient in Dunlop traction.
Wire Configuration
There is some evidence that biomechanically crossed wires are stronger, clinically there is very little difference. The medial pin entry site for crossed pins increases the risk of iatrogenic ulna nerve injury. These injuries are usually due to constriction of the nerve at the cubital tunnel rather than direct penetration with the majority resolving with time.
Risk of iatrogenic ulna nerve injury is increased if the medial wire is inserted when the elbow is hyper flexed rather than extended:
- Medial wire inserted in hyperflexion 15%
- Medial wire inserted in extension 4%
- Lateral wires alone 0%
Two lateral pins
Perform and confirm stability
Pin separation should be enough to allow pins to engage both medial and lateral columns
Two rather than three wires is usually sufficient for stable fractures. Unstable may require a third wire or a medial wire.
Two crossed pins
Biomechanically strongest to torsional stress
Higher risk of ulnar nerve injury (4-15%)
Highest risk if placed with elbow in hyperflexion (15%)
Blind, percutaneous medial wire insertion has a higher risk than mini-incision and blunt dissection
Technique
- If a medial wire is used the lateral wire should be placed first to stabilise the fracture, the elbow extended and then medial wire placed.
- A mini-incision with blunt dissection to the medial surface should be employed if placing a medial wire
- On AP radiograph there should be maximal pin separation at the fracture site (at least >2mm)
- Pins should engage both the medial and lateral column just proximal to the fracture site
- Pins should engage both cortices to ensure stability
References
- Omid, R, Choi PD, Skaggs, DL. Supracondylar Humeral Fractures in Children. J Bone Joint Surg Am. 2008; 90: 1121- 1132.
- Gartland JJ. Management of supracondylar fractures of the humerus in children. Surg Gyn Obstet. 1959; 109:145-154.
- Kocher MS, Kasser JR, Waters PM, et al. Lateral entry compared with medial and lateral entry pin fixation for completely displaced supracondylar humeral fractures in children: a randomized clinical trial. J Bone Joint Surg Am. 2007; 89:706-712.
- Mangat KS, Martin AG, Bache CE. The 'pulseless pink' hand after supracondylar fracture of the humerus in children: the predictive value of nerve palsy. J Bone Joint Surg Br. 2009 Nov;91(11):1521-5.
- Blakey CM, Biant LC, Birch R. Ischemia and the pink pulseless hand complicating supracondylar fractures of the humerus in childhood: long-term follow-up. J Bone Joint Surg Br. 2009; 91:1487-1492.
- White LA, Mehlman CT, Crawford AH. Pulseless and puzzling, vascular injuries in supracondylar humeral fractures in children: a meta-anlaysis of observational studies and results of a POSNA membership survey. J Pediatr Orthop. 2010; 30:328-335