Core Knowledge: Flexor Tendon Sheath Infections

Today’s Wednesday Blog gives an overview of flexor tendon sheath infections, a common exam and interview question.
Background
Flexor tendon sheath infections occur when infectious organisms multiply in the closed space of the flexor tendon sheath. Natural immune response mechanisms cause swelling and migration of inflammatory cells and mediators. The septic process and inflammatory reaction within the tendon sheath interfere with the tendon gliding mechanism, leading to scarring, tendon necrosis, disruption of the tendon sheath and conjecture of the fingers.
Anatomy
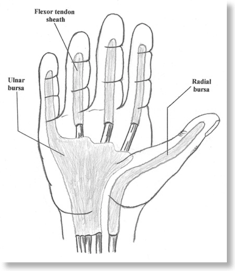
The visceral and parietal layers of the flexor tendons are joined at the ends to produce a closed compartment filled with synovial fluid. Tendon sheaths lie in close proximity to adjacent bursa and infection of the flexor tendons can spread proximally to the hand and wrist. The flexor tendon sheaths of flexor digiti minimi and flexor pollicis are at particular risk of spreading to the ulna and radial bursa respectively.
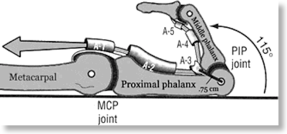
When considering incisions for drainage particular care must be taken with respect to the pullies that facilitate tendon gliding and stability. A2 and A4 being the most important (see diagrams)

Diagnosis
Much of the original work on flexor tendon infections was done by Kanavel.
If a patient presents with the 4 Kanavel signs, flexor tendon infection is diagnosed (see top image also). The 4 Kanavel signs are:
(1) finger held in flexion
(2) fusiform swelling
(3) tenderness along the flexor tendon sheath
(4) pain with passive extension of the digit
The process has the ability to rapidly destroy a finger's functional capacity and is considered an orthopedic emergency.
Management
For patients who are immunocompromised or have diabetes, early surgical intervention is warranted.
If medical treatment alone is attempted, then inpatient observation for at least 48 is indicated.
Surgical drainage is necessary if no obvious improvement has occurred within 12-24 hours.
Classification
The Michon classification helps to guide management at time of surgery
| Infection Stage | Characteristic Findings | Treatment |
| Stage I | Increased fluid in sheath, mainly a serous exudate | Catheter irrigation |
| Stage II | Purulent fluid, granulomatous synovium | Minimal invasive drainage +/- indwelling catheter irrigation |
| Stage III | Necrosis of the tendon, pulleys, or tendon sheath | Extensive open debridement and possible amputation |
Technical Aspects of Surgery
Catheter Irrigation:
Two small incisions are made to allow insertion of a small catheter and irrigation.
The proximal incision is made over the A1 pulley.
If the radial or ulnar bursa is the suggested the incision can be made proximal to the transverse carpal ligament.
The distal incision is made over the region of the A5 pulley.
A 16-gauge polyethylene catheter or pink cannula is inserted into the tendon sheath through the proximal incision. The sheath is copiously
irrigated with a minimum of 500 mL of normal saline. Avoid excessive fluid extravasation into the digit because it can result in necrosis of the digit.
The catheter can be loosely sewn in or simply removed after irrigation. A small drain is placed in the distal incision, and the wounds are left open.
A splint is applied, the hand is elevated, and the appropriate empiric antibiotic coverage is started while awaiting culture results.
Brunner Incision:
A Brunner incision allows better initial exposure but may complicate closure/coverage if skin necrosis ensues and is more likely to interfere with
therapy postoperatively.
Further Info:
Orthobullets